Understanding Liver Cirrhosis: Causes, Symptoms, and Prevention

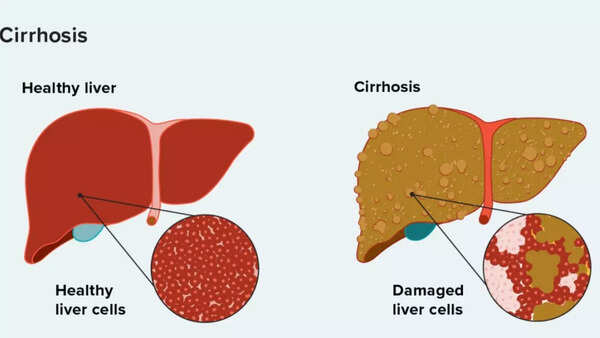
Liver cirrhosis is a serious, long-term disease. It happens when healthy liver cells are slowly replaced by scar tissue. This makes it hard for the liver to do its important jobs, like cleaning toxins from the body and processing nutrients. Common causes include drinking too much alcohol, having hepatitis B or C, and non-alcoholic fatty liver disease. Cirrhosis often doesn’t show symptoms early on, but it can lead to serious problems like liver failure if not treated. This guide will help you understand its causes, symptoms, stages, and how doctors diagnose and treat it. We’ll also talk about why finding it early and making lifestyle changes are so important.
What is Liver Cirrhosis?
Cirrhosis happens when the liver is damaged over a long time, leading to inflammation and scarring. As the liver tries to heal, it forms scar tissue instead of healthy cells. This scar tissue makes the liver stiff, which makes it hard for the liver to do its jobs, like:
- Cleaning toxins from the blood
- Processing nutrients, hormones, and medicines
- Making bile to help with digestion
- Creating proteins for blood clotting and fighting infections
As more scar tissue forms, the liver can’t heal itself anymore. This can eventually lead to end-stage liver disease or liver failure.
Source: Cleveland Clinic
Liver Cirrhosis: Early and Advanced Symptoms
Symptoms can be different depending on how far the disease has progressed. Early signs might be mild, but they get worse as the disease gets worse.
Early Symptoms:
- Feeling tired and weak
- Not feeling hungry or feeling sick to your stomach
- Discomfort in the upper right part of your belly
- Red palms
- Small blood vessels visible on the skin
Advanced Symptoms:
- Yellow skin and eyes (jaundice)
- Dark urine and pale stools
- Itchy skin
- Swollen legs or belly
- Confusion or memory loss
- Bruising and bleeding easily
- Hormonal changes

Liver Cirrhosis: Common Causes
The Cleveland Clinic says cirrhosis is the final result of long-term liver inflammation. Some common causes are:
Drinking Too Much Alcohol
Drinking too much alcohol over time inflames and scars the liver. This can lead to alcoholic hepatitis and eventually cirrhosis.
Non-Alcoholic Fatty Liver Disease (NAFLD)
NAFLD is linked to obesity, high cholesterol, and diabetes. It causes fat to build up in liver cells, which leads to inflammation.
Long-Term Hepatitis B and C Infections
Both of these viral infections attack liver cells, leading to long-term damage and scarring. Hepatitis C often doesn’t show symptoms for years.
Autoimmune and Genetic Conditions
Conditions like autoimmune hepatitis, Wilson disease, and hemochromatosis can also lead to cirrhosis by causing ongoing liver inflammation.
Liver Cirrhosis Stages
Source: Healthline
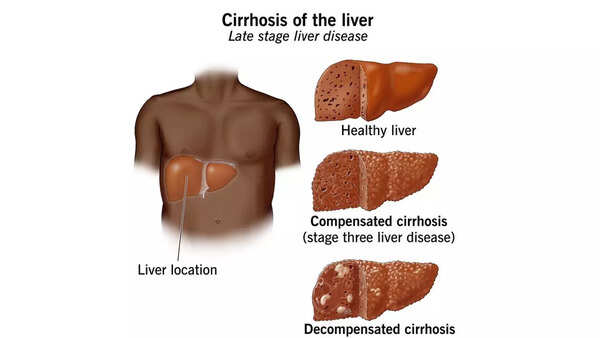
Cirrhosis develops in two main stages, depending on how much the liver has been damaged.
Compensated Cirrhosis
In this early stage, the liver is damaged but can still do its important jobs. Many people don’t have obvious symptoms. Cirrhosis might not be found unless a doctor does blood tests or imaging.
Decompensated Cirrhosis
As scarring gets worse, the liver can’t work well enough. This stage has severe symptoms like jaundice, fluid buildup, bleeding, and mental confusion. This stage can be life-threatening and might need a liver transplant.
How Liver Cirrhosis is Diagnosed
Finding cirrhosis early is important to manage and slow the disease. Doctors might use:
- Blood tests to check liver enzymes, bilirubin, and protein levels
- Imaging tests like ultrasound, CT scan, or MRI to see changes in the liver
- Elastography to check liver stiffness (scarring)
- Liver biopsy to confirm the diagnosis and find the cause
Can Liver Cirrhosis be Cured?
Cirrhosis can’t be reversed, but with the right care, it can be slowed or even stopped. Treatment focuses on managing the cause, improving life quality, and preventing complications.
As cirrhosis gets worse, it can lead to serious and even deadly complications:
- High blood pressure in liver veins (portal hypertension)
- Fluid buildup in the belly (ascites)
- Internal bleeding from enlarged veins (variceal bleeding)
- Liver cancer
- Kidney and lung failure
- Mental confusion or coma
Liver Cirrhosis Diet: What to Eat, What to Avoid
Eat High-Protein Foods
Include lean meats, fish, eggs, beans, nuts, and dairy to help keep your muscles strong and avoid malnutrition.
Eat Both Plant- and Animal-Based Proteins
Eating both supports good nutrition and better liver function.
Avoid Alcohol
Alcohol can make liver scarring worse and make the condition worse.
Limit Processed Foods and Trans Fats
These can increase liver inflammation and cause more damage.
Reduce Salt Intake
Too much salt can cause fluid buildup and swelling.
Avoid Raw or Undercooked Meat and Seafood
Cirrhosis weakens the immune system, increasing the risk of food poisoning.
Managing Cirrhosis Through Nutrition and Medical Support
While cirrhosis can’t be reversed, a liver-friendly diet can slow the disease, ease symptoms, and improve life quality. Getting enough calories, protein, and important nutrients like zinc, vitamin D, and B vitamins is key. However, diet changes can feel hard, especially when avoiding favorite foods like fast food or alcohol. Support from a doctor or dietitian is important to make a plan just for you and ensure you meet your nutritional needs. In some cases, supplements or medicines might also be recommended as part of your treatment.
Cirrhosis of the Liver: Prevention Tips
Cirrhosis usually doesn’t develop overnight—it’s the result of long-term liver damage. While some causes, like genetic disorders, can’t be avoided, many forms of cirrhosis can be prevented through smart lifestyle and healthcare choices. Early action and proactive health monitoring can greatly reduce your risk.
Avoid Alcohol and Illegal Drugs
Alcohol is one of the leading causes of liver cirrhosis, especially when drunk heavily and regularly over time. The liver processes alcohol, and too much can inflame and damage liver cells, leading to scarring.
Keep a Healthy Weight
Being overweight increases your risk of non-alcoholic fatty liver disease (NAFLD), which can lead to cirrhosis if not treated. Obesity-related liver disease is now one of the fastest-growing causes of liver failure worldwide.
What you can do: Eat a nutrient-rich, balanced diet and stay active. Losing even 5–10% of your body weight can reduce liver fat and inflammation a lot.
Get Vaccinated Against Hepatitis B
Hepatitis B is a viral infection that can become long-term and cause ongoing liver inflammation and damage. It is a major cause of cirrhosis worldwide.
Manage Diabetes, Cholesterol, and Blood Pressure
Conditions like type 2 diabetes, high cholesterol, and high blood pressure are linked to fatty liver disease and cirrhosis.
What you can do: Regularly check your blood sugar and cholesterol levels. Follow your doctor’s advice on diet, exercise, and medicine to keep these risk factors in check.
Get Regular Liver Checkups if You Are at Risk
Many people with early-stage liver damage don’t have symptoms. That’s why routine screenings can save lives, especially for people who have:
- A history of heavy alcohol use
- Long-term hepatitis B or C
- Obesity or diabetes
- A family history of liver disease
What you can do: Ask your healthcare provider for periodic liver function tests or imaging scans if you’re in a high-risk group.

Living with Cirrhosis: Daily Tips for Better Management
If you’ve been diagnosed with cirrhosis, there’s still a lot you can do to slow its progression and keep your quality of life. Medical care combined with healthy lifestyle habits can help you manage symptoms and avoid complications.
Follow a Liver-Friendly Diet
- Your liver is central to digestion and metabolism, so supporting it with the right nutrition is important.
- Eat plenty of fruits, vegetables, lean proteins, and whole grains
- Limit salt to reduce fluid buildup
- Avoid raw or undercooked shellfish, which may carry harmful bacteria
Avoid Alcohol and Harmful Medicines
Even small amounts of alcohol can make liver damage worse once cirrhosis is present. Some over-the-counter medicines, especially acetaminophen and NSAIDs (like ibuprofen), can also strain the liver. Always talk to your doctor before taking any new medicine, supplement, or herbal remedy.
Take Prescribed Medicines Regularly
Medicines might be prescribed to treat the cause of liver damage (e.g., antivirals for hepatitis, diuretics for fluid buildup, or lactulose for mental confusion).
Consistency is key—don’t skip doses and tell your doctor about any side effects.
Watch for Warning Signs of Complications
Cirrhosis can cause sudden complications, so it’s important to stay alert. Contact your doctor if you notice:
- Belly swelling
- Confusion, drowsiness, or personality changes
- Bleeding, bruising, or dark tarry stools
- Sudden weight gain or loss
Stay Connected to Your Care Team
Regular check-ups with a liver doctor or stomach doctor are vital. Your doctor will check your liver function, look for complications like enlarged veins or liver cancer, and adjust your treatment as needed. You might need regular blood tests, ultrasounds, or endoscopies.
Disclaimer: This article is for general information and education only. It’s not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions about liver cirrhosis or any other medical condition.


